By Dr. Aswin Babu
Edited by Dr. Ahmed El-Medany
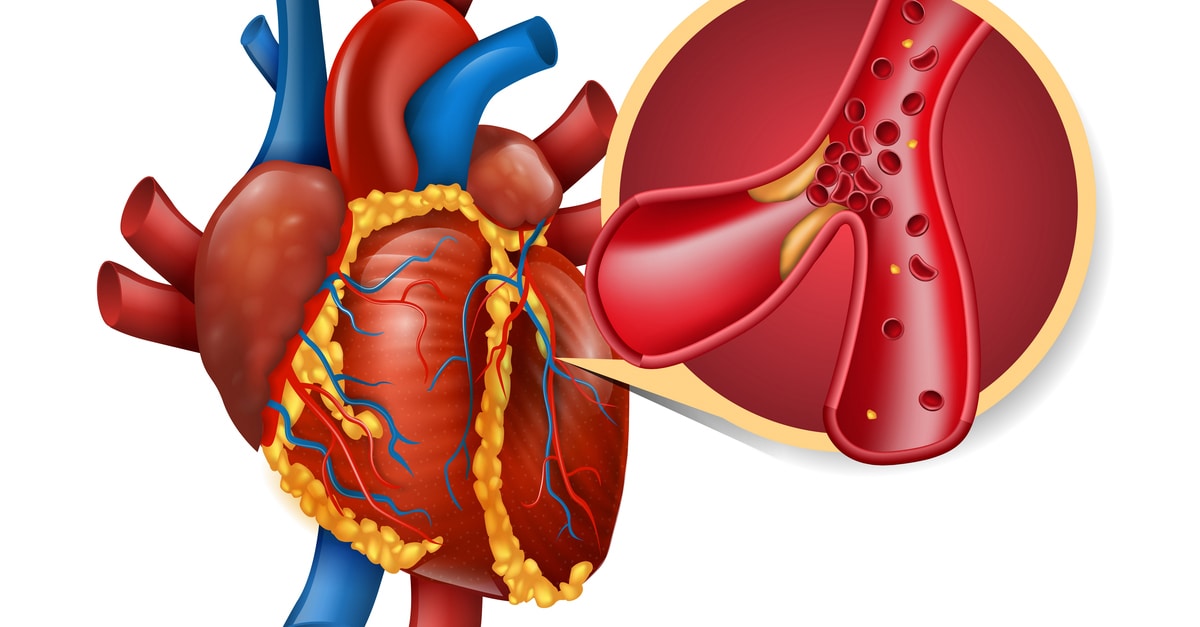
The FIRE trial brings forth strong evidence for a transformative approach in managing older patients presenting with acute myocardial infarction (MI) accompanied by multivessel coronary artery disease (CAD). This trial assessed whether multivessel revascularization guided by coronary physiology over the conventional culprit-only revascularisation strategy would show a benefit in hard cardiovascular outcomes.
The trial was a randomised, parallel, open-label study design. Among the enrolled patients (n=1,445), 720 underwent multivessel revascularisation guided by coronary physiology, while 725 received culprit-only revascularisation. It is important to note the patients were randomised to either group after successful percutaneous coronary intervention (PCI) to the culprit lesion.
Inclusion criteria for participation were well-defined: patients had to be aged 75 years or older and diagnosed with either ST-segment elevation myocardial infarction (STEMI) or non-ST-segment elevation myocardial infarction (NSTEMI). Exclusion criteria included patients with an unclear culprit lesion, a life expectancy < 1 year, or a history of prior coronary artery bypass grafting (CABG).
Patients were followed-up for a duration of 12 months. Impressively, the median age of participants was 80 years (77-84), with 37% being females and 32% having a diagnostic label of diabetes. Notably 509 patients (35.2%) presented as a STEMI.
The primary outcome was a composite of major adverse cardiovascular events (MACE) (death, MI, stroke, or ischemia-driven revascularisation). The results were remarkably positive for physiology-guided multivessel PCI. Composite MACE occurred in 15.7% of the physiology-guided complete revascularisation arm compared to 21.0% in the culprit-lesion only cohort (p = 0.01). More impressively, individual endpoints of MACE including death, MI, and revascularisation were all statistically significant in favour of complete revascularisation.
Secondary outcomes of cardiovascular death or MI was notably lower at 8.9% in the physiology-guided complete revascularisation group compared to 13.5% in the culprit-lesion only arm (p < 0.05). Intriguingly, the safety end points of acute kidney injury, stroke, or major bleeding displayed no significant differences between the 2 treatment groups.
The FIRE trial shines a light on a promising avenue for enhancing patient outcomes in older individuals with acute MI. The adoption of physiology-guided complete revascularisation demonstrates clear advantages over the conventional culprit-lesion only approach. Crucially, this shift in strategy is not accompanied by an increased risk of acute kidney injury, stroke, or major bleeding. This is likely secondary to the beneficial information provided by physiology which resulted in 50.9% of non-culprit lesions not undergoing PCI.
However, some limitations do exist such as the bias of randomisation after culprit PCI was performed. This could randomise more diffuse, complex, non-attractive lesions into the medical arm resulting in higher MACE outcomes. Still, these findings align with the growing body of evidence supporting the implementation of comprehensive revascularisation strategies.
Link to Article – https://www.nejm.org/doi/full/10.1056/NEJMoa2300468