The latest updates from the UK and globally on COVID-19 with relevance to cardiology.
- Application of artificial intelligence to the electrocardiogram
By ZI Attia et al
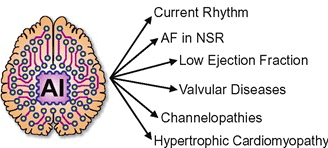
Taken directly from the European Heart JournalArtificial intelligence (AI) has given the electrocardiogram (ECG) and clinicians reading them super-human diagnostic abilities. Trained without hard-coded rules by finding often subclinical patterns in huge datasets, AI transforms the ECG, a ubiquitous, non-invasive cardiac test that is integrated into practice workflows, into a screening tool and predictor of cardiac and non-cardiac diseases, often in asymptomatic individuals.
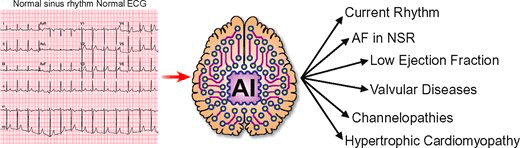
This review describes the mathematical background behind supervised AI algorithms, and discusses selected AI ECG cardiac screening algorithms including those for the detection of left ventricular dysfunction, episodic atrial fibrillation from a tracing recorded during normal sinus rhythm, and other structural and valvular diseases. The ability to learn from big data sets, without the need to understand the biological mechanism, has created opportunities for detecting non-cardiac diseases as COVID-19 and introduced challenges with regards to data privacy. Like all medical tests, the AI ECG must be carefully vetted and validated in real-world clinical environments.
Finally, with mobile form factors that allow acquisition of medical-grade ECGs from smartphones and wearables, the use of AI may enable massive scalability to democratise healthcare.
Read full article here: https://academic.oup.com/eurheartj/advance-article-abstract/doi/10.1093/eurheartj/ehab649/6371908
References:
Zachi I Attia, David M Harmon, Elijah R Behr, Paul A Friedman, Application of artificial intelligence to the electrocardiogram, European Heart Journal, 2021;, ehab649, https://doi.org/10.1093/eurheartj/ehab649 - RCP release statement on COVID-19 vaccination for the severely immunosuppressed
On the 13th of September the Royal College of Physicians (RCP) released a statement regarding vaccination in the severely immunocompromised, in response to the Joint Committee on Vaccination and Immunisation (JCVI) advice that a third COVID-19 vaccination would be offered to ‘severely immunosuppressed people’.
The statement covers JCVI advice regarding which vaccine to administer, as well as guidance on identifying severely immunosuppressed individuals by medical specialty. Of note, those who are severely immunosuppressed will not be able to self-refer for a third primary vaccination, and may require a letter confirming their requirement for a third dose.
Details of the RCP policy, as well as a PDF of their statement, can be found here
- Inequalities in Health Alliance calls on Prime Minister to reduce health inequalities.

92 senior representatives of the Inequalities in Health Alliance (IHA) have written to the Prime Minister calling for a cross-government strategy to reduce health inequalities.
The letter makes calls for a cross-government health inequalities strategy with clear measurable goals, that consider the role of every department and every available policy lever.

Health inequality was a problem before COVID-19 – with a gap in healthy life expectancy between the richest and poorest areas of around 19 years – but the pandemic has tragically demonstrated how these inequalities can have an impact in just a matter of weeks.
The Inequalities in Health Alliance (IHA), first called for a cross-government strategy to reduce health inequalities when it launched in October 2020
The IHA is a coalition of nearly 80 organisations, including the British Cardiovascular Society, launched to press for urgent action to address health inequalities.
References
- Danger: High levels of hospital bed occupancy rates in England

Taken directly from BMJ news
- Overall, 83.8% of the 123 707 beds available overnight were occupied between April and June this year, show bed occupancy rates data from NHS England.
- 82 trusts exceeded the 85% rate which is generally considered to be the limit at which hospitals are able to work safely and effectively.
- 35 of these trusts had reached occupancy levels above 90%, while six trusts reached levels above 95%.
- “Hospitals will experience capacity pressures at lower overall occupancy rates than would previously have been the case.”
- NHS has lost more than 4500 general and acute beds compared with before the pandemic, because of the need for stringent COVID-19 infection control measures.
Read full article: https://www.bmj.com/content/374/bmj.n2079.full
Read related: https://www.bmj.com/content/374/bmj.n2079/rapid-responsesReference:
O’Dowd A. Hospital bed occupancy rates in England reach dangerously high levels. BMJ. 2021 Aug 20;374:n2079. doi: 10.1136/bmj.n2079. PMID: 34417251. - Guidance for Health Care Leaders During the Recovery Stage of the COVID-19 Pandemic

A Consensus Statement
Taken directly from JAMA Network OpenQuestion
What leadership imperatives are most essential for health leaders following the emergency stages of the COVID-19 pandemic?
Findings
In this consensus statement, 32 co-authors from 17 countries with expertise in various aspects of health leadership, health care, public health, and related fields outline 10 imperatives to guide leaders through recovery from the emergency stages of the pandemic. Key leadership capabilities and reflection questions are presented to guide leaders and to structure performance reviews.
Meaning
Leaders who most effectively implement this framework are ideally positioned to address urgent needs and inequalities in health systems and to co-create a culture within their organizations that best serves its people.
The 10 imperatives
- Acknowledge staff and celebrate successes
- Provide support for staff well-being
- Develop a clear understanding of the current local and global context, along with informed projections
- Prepare for future emergencies (personnel, resources, protocols, contingency plans, coalitions, and training)
- Reassess priorities explicitly and regularly and provide purpose, meaning, and direction
- Maximise team, organisational, and system performance and discuss enhancements
- Manage the backlog of paused services and consider improvements while avoiding burnout and moral distress
- Sustain learning, innovations, and collaborations, and imagine future possibilities
- Provide regular communication and engender trust
- In consultation with public health and fellow leaders, provide safety information and recommendations to government, other organisations, staff, and the community to improve equitable and integrated care and emergency preparedness systemwide.
Read full article:
https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2781729
Reference:
Geerts JM, Kinnair D, Taheri P, Abraham A, Ahn J, Atun R, et al. Guidance for Health Care Leaders During the Recovery Stage of the COVID-19 Pandemic: A Consensus Statement. JAMA Netw Open. 2021 Jul 1;4(7):e2120295. doi: 10.1001/jamanetworkopen.2021.20295. PMID: 34236416. - Anticoagulation of Patients with Mechanical Heart Valves.

The British Cardiovascular Society (BCS) has today released a Joint Statement together with the British Heart Valve Society (BHVS), the Society for Cardiothoracic Surgeons (SCTS), the British Society of Echocardiography (BSE), the Primary Care Cardiovascular Society (PCCS) and the British Congenital Cardiac Association (BCCA) on Anticoagulation of Patients with Mechanical Heart Valves.
On 14 July 2021, a National Patient Safety Alert was issued by NHS England relating to choice of anticoagulant drugs prescribed to patients with mechanical heart valves. [1] This was triggered by cases presenting to hospital of patients who had been switched from anticoagulation with warfarin to a novel oral anticoagulant (NOAC).
As a result of the Coronavirus pandemic and the national lockdown in 2020, some patients experienced significant difficulty in continuing blood monitoring of the international normalised ratio (INR). Thus, guidance was provided for patients who could be safely switched from warfarin to newer oral anticoagulant drugs – this did not include patients with mechanical heart valves. [2]
The NPSA stated that fourteen patients with mechanical heart valves have been identified who had been switched from warfarin to alternative anticoagulant drugs – one patient was switched to a low molecular weight heparin (LMWH) and thirteen patients to a NOAC. On subsequent analysis of patient records in primary care, a further 750 patients have been identified who are coded as having a mechanical heart valve and prescribed a NOAC.
- Clinical outcome of COVID-19 in patients with adult congenital heart disease
By Saadia Aslam
Original research from Professor Markus Schwerzmann and his team collected clinical outcome data to help identify risk factors for a complicated course of COVID-19 (defined as: hospitalisation requiring non-invasive or invasive ventilation and/or inotropic support, or a fatal outcome) in patients with adult congenital heart disease. Twenty-five centres from nine different European countries participated in the study and recruited consecutive ACHD patients diagnosed with COVID-19 between 27 March and 6 June 2020.
The results showed that of 105 patients with a mean age of 38±13 years (58% women), 13 had a complicated disease course, of whom 5 died. In univariable analysis, age (OR 1.3, 95% CI 1.1 to 1.7, per 5 years), ≥2 comorbidities (OR 7.1, 95% CI 2.1 to 24.5), body mass index of >25 kg/m2 (OR 7.2, 95% CI 1.9 to 28.3) and cyanotic heart disease (OR 13.2, 95% CI 2.5 to 68.4) were associated with a complicated disease course. In a multivariable logistic regression model, cyanotic heart disease was the most important predictor (OR 60.0, 95% CI 7.6 to 474.0).
In this patient group, general risk factors such as; age, obesity and multiple comorbidities are associated with an increased risk of complicated COVID-19 course. However, cyanotic lesions, including unrepaired cyanotic defects or Eisenmenger syndrome were at particularly high risk.
Reference
Schwerzmann M, Ruperti-Repilado FJ, Baumgartner H, Bouma B, Bouchardy J, Budts W, et al. Clinical outcome of COVID-19 in patients with adult congenital heart disease. Heart. 2021 Mar 8:heartjnl-2020-318467. doi: 10.1136/heartjnl-2020-318467. Epub ahead of print. PMID: 33685931; PMCID: PMC7944416. - Myocarditis recognised rare adverse association with COVID-19 vaccine

By Ahmed El-Medany
In a case series of 23 male patients, by Montgomery et al (2021), myocarditis was identified within 4 days of administration of a COVID-19 vaccine.
20 out of 23 of these patients received a diagnosis of myocarditis following their second dose of mRNA COVID-19 vaccine. It is important to note that these episodes occurred against a backdrop of 2.8 million delivered doses of mRNA COVID-19 vaccine in the United States.
Furthermore, a case series by Rosner et al (2021) in Circulation, as reported on seven male patients (aged 19-39 years) who developed myocarditis-like symptoms after receiving their COVID-19 vaccination. Five received Pfizer/BioNTech’s mRNA vaccina, one received Moderna’s mRNA vaccina, and one received Johnson & Johnson’s non-mRNA vaccine. All symptoms resolved by hospital discharge; the mean length of hospital stay was 3 days.
In a related press release, the American Heart Association has stated that reports of vaccine-induced myocarditis should not dissuade people from getting vaccinated. “The American Heart Association continues to urge all adults and children ages 12 and older in the U.S. to receive a COVID-19 vaccine as soon as they can, as recommended by the CDC. Research continues to indicate that the COVID-19 vaccines are 91% effective at preventing severe COVID-19 infection and spreading the virus to others. In addition, the benefits of vaccination far exceed the very unusual risks,” the AHA said in the release.
“According to the CDC, fewer than 1,000 cases of myocarditis-like illnesses were reported as of May 31, 2021, and nearly 312 million doses of COVID-19 vaccines have been administered in the U.S. to date.”
More here:
Myocarditis Following Immunization With mRNA COVID-19 Vaccines in Members of the US Military | JAMA Cardiology | JAMA Network
Myocarditis Temporally Associated with COVID-19 Vaccination | Circulation (ahajournals.org) - COVID-19 and Cardiology ARCP outcomes: a summary for trainers and trainees

By Ahmed El-Medany
Disruption to training due to the COVID-19 pandemic has led to difficulties for some trainees in acquiring the competencies required to progress, or complete, their training.
However, where the acquisition of competencies has been delayed due to COVID-19 and there are no serious concerns about the trainee, one of the two new ARCP outcomes, Outcome 10.1 or Outcome 10.2 have been suggested by the Statutory Education Bodies (SEBs) of the 4 Nations.
The aim of introducing these new ARCP outcomes has been to enable trainees to progress or complete their training programme where possible. Of note TPDs, and the ARCP panels they lead, have the discretion to make ‘common sense’ decisions for trainees. The usual outcomes (1,2, and 3) will also be available and awarded as usual.
ARCP Outcome 10.1
Outcome 10.1 recognises that the trainee has been making progress in their training but there has been delay in the acquisition of competencies/capabilities due to COVID-19, and the trainee is likely to be able to acquire these capabilities without the need for extra training time. An Outcome 10.1 may be awarded at different stages of Cardiology training.ARCP Outcome 10.2
Outcome 10.2 recognises that the trainee has been making progress in their training, and there is a delay in the acquisition of competencies due to COVID-19. Therefore, it either would not be safe or not possible for the trainee to progress in, or complete, their training programme and additional training time is required. For trainees approaching certification, trainees may be able to act up as a consultant (AUC) and acquire their missing capabilities during their additional training time where this facility exists in the curriculum.We interviewed Dr. Alison Calver, JRCPTB Cardiology Specialist Advisory Committee Chair, BCS Vice-President for Training, and Consultant Interventional Cardiologist at University Hospital Southampton. She kindly provided us with the following information about modifications to the Cardiology ARCP decision aid, in the context of the COVID-19 pandemic:
Modifications to Cardiology ARCP decision aid in Covid 19 pandemic 2021
‘The Cardiology decision aid is very comprehensive. It should be used in conjunction with the ARCP guidance for the use of Covid outcomes (10.1, 10.2; Mike Jones slide) and the following recommendations:
- ST3s who are behind due to COVID at 2021 summer’s ARCP can probably catch up over 5 years.
- ST4s who are significantly behind due to COVID at 2021 summer’s ARCP may not be able to catch up without undue pressure being heaped on Trainee. Therefore, TPDs should consider 10.2.
- At ST5: Echo (BSE or curriculum tool) needs to be completed. They may need 10.2 if this is not the case. Near completion e.g. video cases only outstanding. TPD discretion is required whether this can be made up during Advanced Module 2 years
- At ST5: some latitude around level 3 angiography for those that do not wish to do PCI. Consider simulation if level 3 DOPS required.
- At ST5: some latitude if core ACHD, ICVD, MRI, CT, Nuclear not signed off, provided Advanced Module choice does not include these. No more than 3 of these should be outstanding otherwise the burden to make them up in Advanced Modular training will be too much for trainee.
- At ST7: temp pacing and pericardiocentesis – heavy reliance on simulation except for those pursuing cath lab based Advanced Modules e.g. PCI, EP, Devices.
- All patient surveys, teaching observations, audit assessments, MSFs, patient feedback, management course can be deferred. All can be done at any time during training (unless TPD feels there is a good reason that these need to be done now).
- ALS – to be done at first opportunity post-pandemic, should not hold up a CCT.
- Trainees on OOPR or academic trainees: all are likely to require 10.2 unless very close to finishing as all were re-deployed to clinical duties in pandemic.’
‘Moreover, it is impossible to predict every single scenario with which a trainee might present. However, the guidance is well understood by TPDs and will help trainees get a fair outcome for their personal situation. There is no ‘one size fits all’ and each trainee will get an individualised decision.’
For how long will outcomes 10.1 and 10.2 planned to be used?
No idea. Definitely for 2021.What support mechanisms can supervisors direct their trainees to following an Outcome 10.1/10.2?
These will be personalised to individual trainees. Different solutions will work in different localities.For trainees dual accrediting with GIM, that were redeployed to general medicine and completed their relevant competencies, is there a potential plan for allocating more training time to cardiology later in their training (i.e. ST7) and avoiding more GIM commitment?
Training skills of any sort (GIM, leadership, management etc) acquired during re-deployment can (and should) count towards CCT. It is important that trainees record it in e-portfolio and acquire the appropriate WPBA to provide evidence of their training. This advice was given to trainees via the SAC/BJCA in March 2020.JRCPTB ARCP information hub: COVID-19 | JRCPTB
- Greater adverse outcomes in patients presenting with COVID-19 and STEMI
Outcomes from the North American COVID-19 STEMI registry
The goal of the NACMI (North American COVID-19 and STEMI) registry is to describe demographic characteristics, management strategies, and outcomes of COVID-19 patients with STEMI.
Methods
A prospective, ongoing observational registry was created under the guidance of 3 cardiology societies.
Group 1: STEMI patients with confirmed COVID+
Group 2: suspected COVID-19 infection
Group 3: Control group that was age- and sex-matched STEMI patients (matched to COVID+ patients in a 2:1 ratio) treated in the pre-COVID era (2015 to 2019)The primary outcome was a composite of in-hospital death, stroke, recurrent myocardial infarction, or repeat unplanned revascularization.
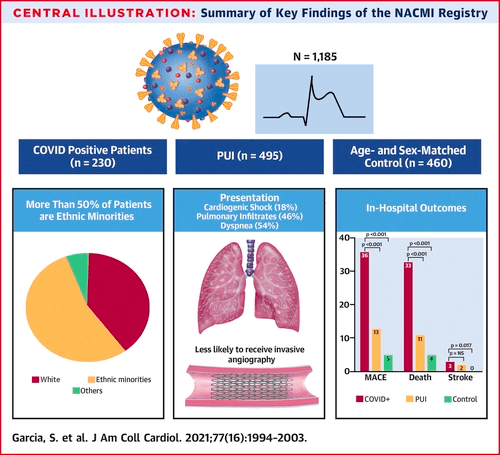
Key findings of the NACMI Registry Results
As of December 6, 2020, 1,185 patients were included in the NACMI registry (230 COVID+ patients, 495 PUIs, and 460 control patients).- COVID+ patients were more likely to have minority ethnicity (Hispanic 23%, Black 24%) and had a higher prevalence of diabetes mellitus (46%) (all p < 0.001 relative to PUIs).
- COVID+ patients were more likely to present with cardiogenic shock (18%) but were less likely to receive invasive angiography (78%) (all p < 0.001 relative to control patients).
- Among COVID+ patients who received angiography, 71% received PPCI and 20% received medical therapy (both p < 0.001 relative to control patients).
- The primary outcome occurred in 36% of COVID+ patients, 13% of PUIs, and 5% of control patients (p < 0.001 relative to control patients).
Conclusions
COVID+ patients with STEMI represent a high-risk group of patients with unique demographic and clinical characteristics. PPCI is feasible and remains the predominant reperfusion strategy, supporting current recommendations.Read more:
https://www.jacc.org/doi/10.1016/j.jacc.2021.02.055Editorial Comment:
https://www.jacc.org/doi/10.1016/j.jacc.2021.03.231 - ACC and AHA release key data elements and definitions for heart failure

By Ahmed El-Medany
On 23 March, the American College of (ACC) and American Heart Association (AHA) released the 2021 ACC/AHA Key Data Elements and Definitions for Heart Failure in the Journal of the American College of Cardiology.
This new document, led by writing committee co-chairs Bozkurt and Hershberger, supersedes the previous 2005 clinical standards, and includes data elements for heart failure (HF) risk factors, cardiovascular history, and non-cardiovascular health determinants, including COVID-19 infection.
Other highlights include an updated patient assessment with more detailed elements for symptoms, signs, clinical exam findings, stages, and functional assessment.
The full clinical data standards can be found at
https://www.jacc.org/doi/10.1016/j.jacc.2020.11.0Biykem Bozkurt, Ray E. Hershberger, Javed Butler, Kathleen L. Grady, Paul A. Heidenreich, Maria Lizza Isler, James K. Kirklin, and William S. Weintraub
J Am Coll Cardiol. Mar 23, 2021. Epublished DOI: 10.1016/j.jacc.2020.11.012 - Application of Machine Learning to X-Ray and CT images in the diagnosis of COVID-19
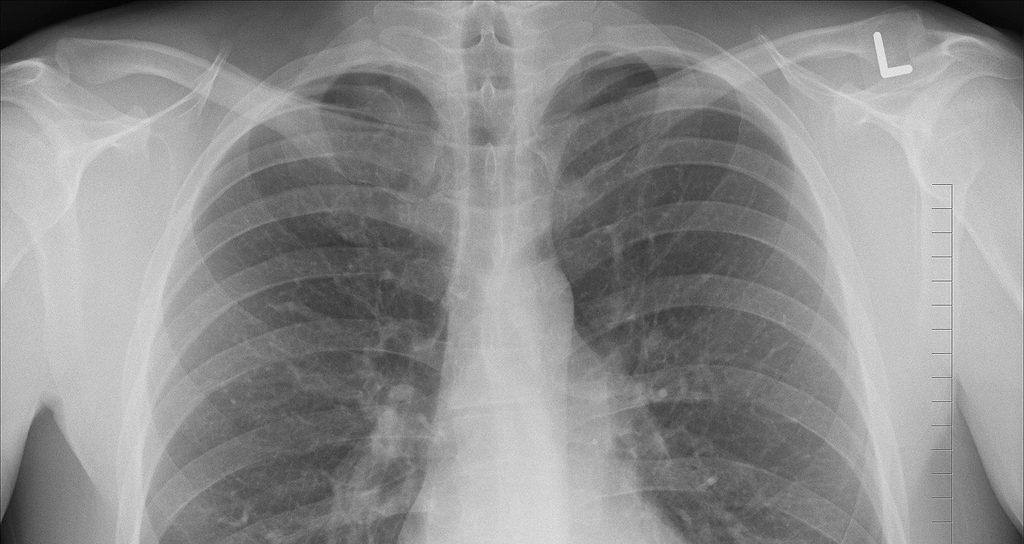
By Ahmed El-Medany
Chest CT scans and X-ray images have been reported to have sensitivity values of 98 and 69%, respectively, with regards to diagnosing SARS-CoV-2 pneumonitis.
In this review by Mohammad-Rahimi et al, 105 studies reporting on machine and deep learning methods on CT and X-ray images in COVID-19 were analysed and compared. The accuracy of these methods ranged from 76% to more than 99%, suggesting the applicability of machine and deep learning methods in the clinical diagnosis of COVID-19; albeit with the requirement for multidisciplinary approaches in cases of clinical uncertainty.
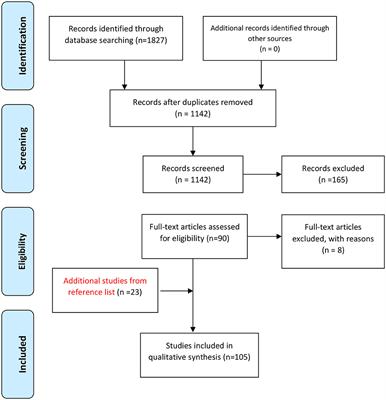
Figure 1. PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) chart showing the process of systematic identification, screening, and selection of articles. Read the full article at: https://www.frontiersin.org/articles/10.3389/fcvm.2021.638011/full#h1
Mohammad-Rahimi, H., Nadimi, M., Langeroudi, A.G., Taheri, M. and Ghafouri-Fard, S., 2021. Application of Machine Learning in Diagnosis of COVID-19 through X-Ray and CT Images: A Scoping Review. Frontiers in Cardiovascular Medicine, 8, p.185. https://doi.org/10.3389/fcvm.2021.63801
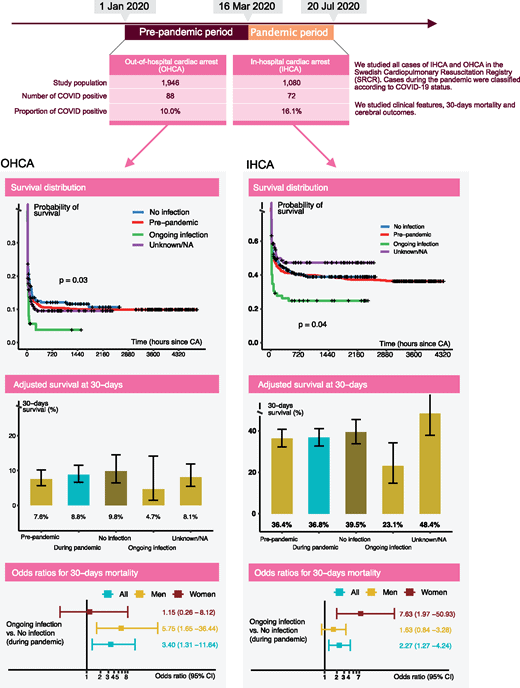
- People infected with COVID-19 have a higher risk of dying after a cardiac arrest. A report from the Swedish Registry for Cardiopulmonary Resuscitation
COVID-19 patients who suffer a cardiac arrest either in or out of hospital are far more likely to die than patients who are not infected with the coronavirus. Women are are nine times more likely to die after suffering a cardiac arrest in hospital, according to Sultanian et al.
This Swedish study showed that COVID-19 was implicated in at least 10% of all out of hospital cardiac arrest (OHCA) and 16% of in hospital cardiac arrests (IHCA). Coronavirus patients who had an OHCA or IHCA had a 3.4 and 2.3-fold increased risk of dying within 30 days, respectively. Unfortunately, none of these patients had been discharged alive from hospital by the time the study was written in October 2020.
- NICE report on the impact cardiovascular disease management

The National Institute for Health and Care Excellence (NICE) has today published a report highlighting progress made by the health and care system in implementing NICE guidance on cardiovascular disease (CVD) management. Alongside the report, Prof Simon Ray, President of the British Cardiovascular Society, provides insights on the key findings about our role in improving outcomes for people with CVD.
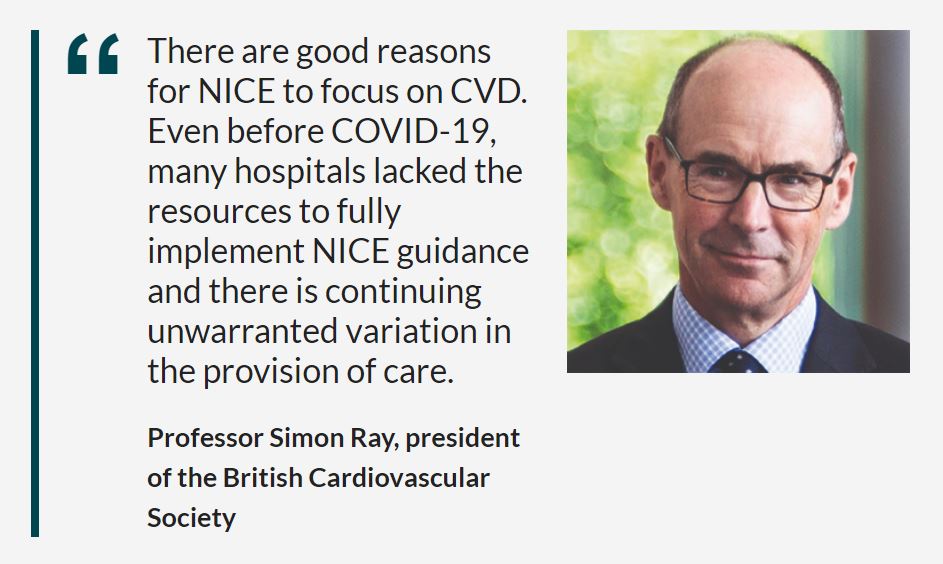
NHS England’s Long Term Plan suggests that CVD is the main area in which the NHS can save lives over the next 10 years.
- 6 million people live with CVD
- £7.4 billion estimated annual healthcare costs
- 120,000 people died from diseases of the circulatory system in 2019
- 56% decrease in the rate of deaths from treatable diseases since 2000
Most of the data refers to the impact of NICE guidance before COVID-19, but the report does include some data collected during the pandemic, highlighting some of the different ways that care has been delivered.
Key findings from the report
Read a summary of the findings
For more detailed information, download the full report from the NICE website.
- Leading cardiovascular organisations call for urgent action to reduce air pollution

“Even before the COVID-19 pandemic, air pollution was an issue of growing concern due to its impact on people’s health, although it was frequently overlooked as a risk factor for cardiovascular disease. COVID-19 has brought a new, deadly factor to the equation, and the time has come for the health community to speak up and take action,” – Michael Brauer, Chair of the World Heart Federation Air Pollution Expert Group.
The World Heart Federation (WHF), American College of Cardiology (ACC), American Heart Association (AHA) and European Society of Cardiology (ESC) – today released a joint statement urging the medical community and health authorities to mitigate the impact of air pollution on people’s health.
While calling for structural actions to reduce emissions of air pollutants and harmful exposure, the statement also highlights the important role that healthcare providers play in preventing illnesses related to air pollution, including:
- Advocating for air pollution mitigation as a health measure, further research on air quality and its impact on CVD, and interventions to reduce air pollution and its effect on NCDs
- Providing patients with personal measures to reduce exposure, such as room air filtration systems
- Integrating air pollution into disease management approaches, for example through the use of air quality indices
- Participating in the development of guidelines on air pollution and CVD
- Supporting ministries of environment, energy, and transportation in their mitigation efforts
- Working to educate and raise awareness on the cardiovascular benefits of clean air
- Collaborating with senior decision-makers in national, regional, and global governmental institutions to make air pollution related heart disease a priority
- COVID‐19, myocarditis, and the other side of the bed

Emer Joyce speaks about the impact COVID-19 has had on the clinical landscape of acute cardiac, intensive care and cardiomyopathy/heart failure services including the wide spectrum of newly proposed inflammatory cardiac syndromes, triggered by the severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2).
“If myocarditis is and has always been a chameleon of cardiology, then SARS‐CoV‐2 myocarditis may go on to be its pinnacle.”
In the article, Emer shares an interesting perspective as that of both a subspecialist in the field and of her experience as a patient of SARS‐CoV‐2 myocarditis presenting “a birds‐eye view of the physician as patient, the sub‐specialist as sub‐specialist condition sufferer, the one on the far side of the bed as the one in the bed.”
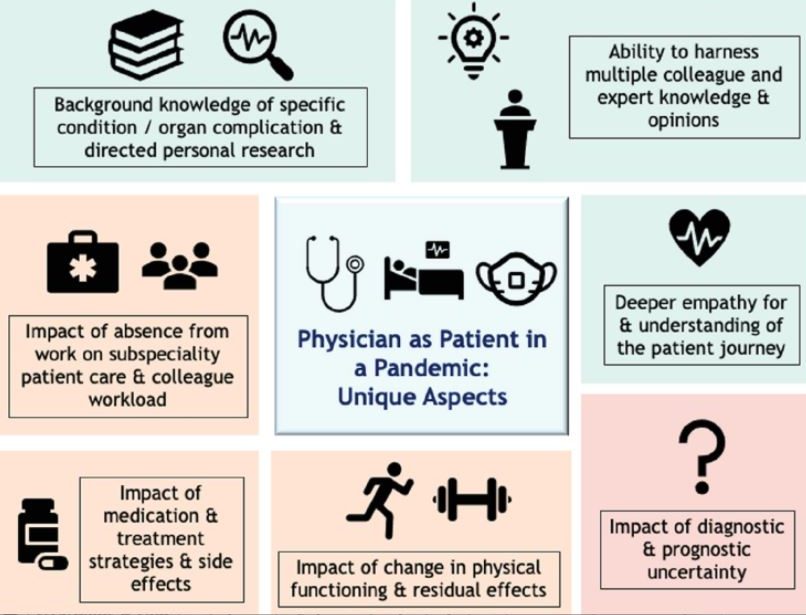
Credit: Emer Joyce
Unique aspects of the physician as patient in a pandemic. Potential less adverse aspects of the physician as patient are highlighted in green, expected more negative and/or compounded impacts of physician as patient are highlighted in shades of orange and red.She speaks of her experience as a patient, with no sub‐specialists in SARS‐CoV‐2 myocarditis to call on of her gratitude to mentors, colleagues, and bona‐fide experts in the fields of cardiology, heart failure/transplant, cardiac imaging, immunology and infectious diseases, both nationally and internationally, of whom she was able to reach out to and obtain wisdom, empathy and reassurance.
Emer highlights that in her experience, rather than ‘knowing it all’ patients place a much higher importance on needing their physicians “to care enough to reach out, call, debate and discuss, on a backdrop of clinical accountability, empathy and respect.“
- BSH position statement on the roll out of COVID-19 vaccinations

Read the BSH position statement on the roll out of COVID-19 vaccinations
The BSH has recently released a statement regarding COVID-19 vaccinations.
The statement advises:
‘Two COVID-19 vaccines are now being used in the UK. The Pfizer/BioNTech vaccine was rolled out on 8th December 2020 and the AstraZeneca/Oxford University vaccine was rolled out on the 4th January 2021.
‘Both vaccines have been thoroughly tested in clinical trials. Both vaccines have met the strictest standards of safety, quality and effectiveness set out by the independent Medicines and Healthcare products Regulatory Agency (MHRA). Millions of patients have now received COVID-19 vaccines worldwide and reports of serious adverse effects are very rare.
‘Heart failure specialists can and should reassure their patients that the vaccines are safe and effective.
‘The only group currently advised not to take the vaccine are people with a history of life-threatening allergic reactions (anaphylaxis) to any component of the vaccine. Pregnant women who are classed
as clinically extremely vulnerable can be considered for the COVID-19 vaccine. This decision should be made on an individual basis and with input from their maternity team. ‘It goes on to say:
‘The Moderna vaccine was approved in the UK on 8th January 2021 and will become available in the coming months. Other vaccines are in development and maybe approved in the coming months. All COVID-19 vaccines will be subject to the same strict MHRA standards.’
The BSH recommends:
People with heart failure are at increased risk of severe COVID-19. The British Society for Heart Failure strongly recommends that all those eligible accept vaccination, if offered.
Patients and healthcare professionals should continue to follow government advice to reduce their risk of infection.
Patients should be reassured that heart failure services are open and they should seek help when it is needed.
References:
https://www.nhs.uk/conditions/coronavirus-covid-19/coronavirus-vaccination/coronavirus-vaccine/ - Impact of COVID-19 on the Incidence and Management of Out of Hospital Cardiac Arrest in Patients Presenting with Acute Myocardial Infarction

Abstract
Authors: Muhammad Rashid, Chris P Gale, Nick Curzen, Peter Ludman, Mark De Belder, Adam Timmis, Mohamed O Mohamed, Thomas F Lüscher, Julian Hains, Jianhua Wu, Ahmad Shoaib, Evangelos Kontopantelis, Chris Roebuck, Tom Denwood, John Deanfield, and Mamas A Mamas
This abstract in the Journal of the American Heart Association covers recent studies on the higher rates of Out of Hospital Cardiac Arrest (OHCA), particularly in older women from an Asian background and the higher rate in hospital mortality in England, UK.
Background
Studies have reported significant reduction in acute myocardial infarction (AMI) related hospitalisations during the COVID-19 pandemic. However, whether these trends are associated with increased incidence of Out of Hospital Cardiac Arrest (OHCA) in this population is unknown.
- Cancellation of Cardiac Procedures During COVID-19

BCS Statement
The COVID-19 pandemic has placed immense pressure on the national health service, with frontline hospital services re-organised to handle the surge in cases. This re-organisation has had a wider impact on non-emergency procedures.
The British Cardiovascular Society has issued a statement highlighting the (intended or unintended) implications of cancelling cardiac procedures and sets out its recommendation for the interventions that should take priority as the backlog of procedures is addressed.
(Unintended but Inevitable) Consequences of Cancellation of Cardiac Procedures During the COVID-19 Pandemic.
- COVID-19: Disentangling Ethnicity and Cardiovascular Risk

BCS Editorial
By Ashwin Ajay and Ahmed Adlan
Pneumonia of unknown cause began spreading in Wuhan, China, in late 2019, which led to the discovery of the severe acute respiratory syndrome coronavirus-2 (SARS CoV-2) as the underlying cause.1 SARS CoV-2 virus causes the disease named COVID-19, which has drastically impacted the world in an unprecedented manner. Much research has been conducted to analyse the spread of the virus and to identify potential risk factors associated with transmission and adverse outcomes.
Since the start of the COVID-19 crisis, it became evident that three factors were associated with worse health outcomes; these include age, co-morbidities and male gender.2 However concerns were raised over a possible association between ethnic groups and worse outcomes in COVID-19.3 Consequently, Public Health England published a report on the disparities in risk and outcomes of COVID-19, including ethnicity.4 In this editorial, we aim to discuss the apparent disproportionate impact that COVID-19 has on black and ethnic minorities and the possible underlying factors.
- COVID-19: Significant drop in ACS admissions

News Article
The COVID-19 pandemic has seen a decline in patients admitted with acute coronary syndromes, a report in the Lancet finds.
Reduced admissions with acute coronary syndromes on an unprecedented scale, were reported by a very distinguished group of authors this week in the Lancet. This national data collection exercise demonstrated a 23% reduction in STEMI and a 42% reduction in NSTEMI. Even within hospitals, practice has changed with a drop of more than 75% in cardiac surgery. Although there is some recovery over time, up until the end of May numbers remain significantly reduced compared with 2019. There was no difference in early mortality for those admitted, however, we cannot know the effect this will have in the entire population. Extensive data regarding early and interventional treatments for acute coronary syndromes makes it is almost inevitable that the result will be a higher rate of late presentations, late complications and death at home without intervention. This would be supported by the rise of around 20% in deaths at home noted elsewhere in the same period.
It has never been more important to emphasise that UK cardiology is open for business and patients with symptoms should continue to present rapidly. As a society we need to make this case to the public, to government and to our own organisation; these need to be properly configured to avoid obstructions to care in this new era.
Weekly admissions to acute National Health Service hospital trusts in England with an acute coronary syndrome, by type (Source: The Lancet)
- COVID-19 and Digital Health: From Bed-Side Manner To Web-Side Manner
BCS Editorial
The COVID-19 pandemic has had a massive global impact like no other. The pressure for healthcare services to deliver has been immense. With limited resources, innovative solutions are required to ensure optimal care is given to our patients.
The pandemic has brought into focus the use of technology in healthcare to help protect patients and healthcare workers from the virus, improve efficiency and make healthcare processes become leaner.
This editorial outlines the use of digital health during the pandemic and the long-term lessons we can learn and how can this help the modern cardiologist…
…Eric Topol, an opinion leader in Cardiology and advocate of digital health has warned that the sudden rush to virtual care risks diminishing the quality of clinical care,
‘it’s inexpensive and expedient, but it’ll never be the same as a physical examination with all of its human qualities of judgment and communication’.
We can influence the future of cardiology by sharing innovations during the pandemic. The British Cardiovascular Society have asked members to share innovations by emailing futurecardiology@bcs.com. Virtual healthcare has been rapidly implemented due to COVID-19 and it is likely that it is now here to stay with a larger uptake than ever before. It remains our duty as clinicians to drive forward innovations in digital health for patient and clinician benefit.