By Dr. Timothy Swinn, edited by Dr. Ahmed El-Medany
The MARC-2 study (‘Measuring athlete’s risk of cardiovascular events’) recently published in Circulation has revealed a correlation between increasing exercise intensity and progression of coronary artery disease over 6.3+-0.5 years of follow up1. The MARC-1 study, published in 20172, studied middle-aged/older males and found that the most active group by exercise volume had the highest prevalence of atherosclerotic plaques and highest coronary artery calcium score. This follow-up study invited the same cohort to assess how exercise volume and intensity may affect progression of coronary artery disease, as assessed by CT coronary angiogram (CTCA).
All surviving MARC-1 participants were invited for follow up. 287 asymptomatic males aged between 50-60 years (99% Caucasian) were included in final analyses. They responded to a validated questionnaire about their exercise habits. Activity intensity was recorded using metabolic-equivalent of task (MET) units and exercise volume as MET.hours per week. Intensity was subsequently split into ‘light’, ‘moderate’, ‘vigorous’, and ‘very-vigorous’; and participants were split into tertiles based on increasing proportions of ‘vigorous’ and ‘very-vigorous’ intensity. All participants then underwent non-contrast gated-CT to assess coronary artery calcification (CAC) using the Agatston score, and 284 participants underwent contrast CTCA to quantify and characterise plaques. Plaque progression was quantified using change in CAC score.
CAC score increased or remained static in all participants; however the largest increases were seen in participants with the highest proportion of exercise time spent undertaking ‘very-vigorous’ activities. Time spent performing ‘vigorous’ activities was associated with a lower increase than ‘very-vigorous’ exercise using both linear and logistic regression analyses (Figure 1). Very vigorous intensity exercise was not associated with the absolute increase in number of plaques, but was associated with plaque progression using logistic regression analyses (adjusted Odds Ratio (OR), 1.09 [1.01 – 1.18] per 10% of time spent performing very vigorous exercise; p=0.04), and this was primarily driven by an increase in number of calcified plaques. Exercise volume was not associated with progression of CAC or number of plaques over this time period.
The authors propose a potential mechanism to explain this finding. Namely, catecholamines increase exponentially at higher exercise intensities, leading to increased heart rate and blood pressure. This may lead to turbulent flow and endothelial damage. Additionally, monocytes may undergo long-lasting pro-inflammatory change in the presence of catecholamines. It should be noted, however, that this is not necessarily bad news for athletes as the rate of cardiovascular events remains lower in athletes than non-athletes and the increase in coronary artery disease was primarily driven by increase in more stable, calcified plaques. Further research is required to establish whether there is a causative mechanism for very vigorous exercise leading to coronary artery disease and what the clinical implications may be.
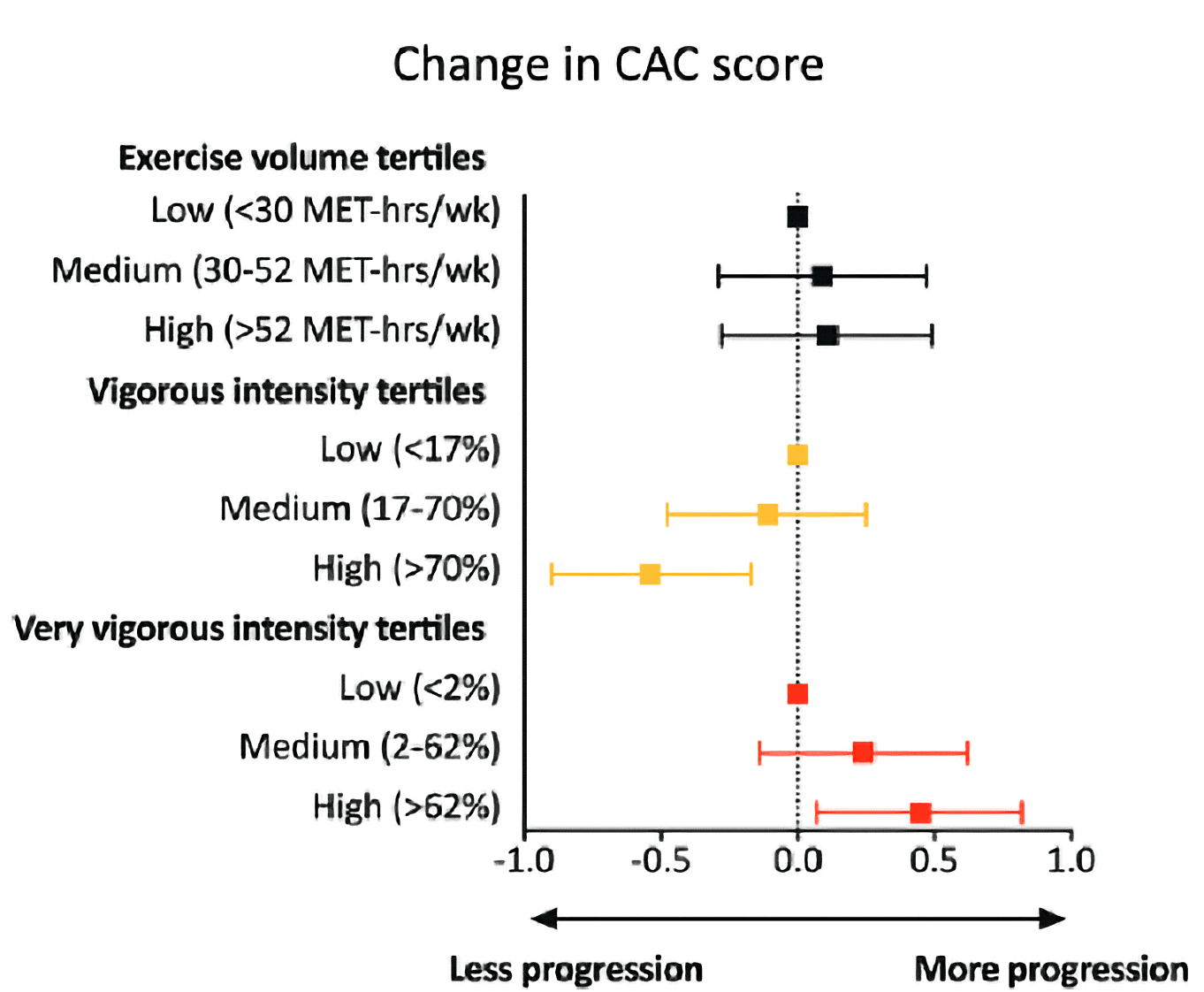
Figure 1: Figure adapted from Aengevaeren et al 20231 shows how vigorous intensity exercise is associated with lower progression of CAC, whereas very-vigorous intensity is associated with more progression
References
- Aengevaeren VL, Mosterd A, Bakker EA, Braber TL, Nathoe HM, Sharma S, et al. Exercise Volume Versus Intensity and the Progression of Coronary Atherosclerosis in Middle-Aged and Older Athletes: Findings From the MARC-2 Study. Circulation [Internet]. [cited 2023 Feb 13];0(0). Available from: https://www.ahajournals.org/doi/10.1161/CIRCULATIONAHA.122.061173
- Aengevaeren VL, Mosterd A, Braber TL, Prakken NHJ, Doevendans PA, Grobbee DE, et al. Relationship Between Lifelong Exercise Volume and Coronary Atherosclerosis in Athletes. Circulation. 2017 Jul 11;136(2):138–48.

