Article by:
Dr Laura Dobson
Consultant Cardiologist, Manchester University NHS Foundation Trust
The Medicines and Healthcare products Regulatory Agency (MHRA) drug safety update:
Systemic and inhaled fluoroquinolones: small risk of heart valve regurgitation; consider other therapeutic options first in patients at risk
This update was published by the MHRA in December 2020, suggesting that oral, intravenous or inhaled fluoroquinolones (FQ’s) are only prescribed after careful benefit-risk assessment and after consideration of other agents in ‘at risk’ patients classified as those with pre-existing congenital or degenerative valve disease, connective tissue disease or those with risk factors for valve dysfunction (such as hypertension, Turners syndrome, Behcets, rheumatoid arthritis and infective endocarditis). The update also states that if ‘at risk’ patients are prescribed FQs they should be counselled regarding the importance of seeking medical attention should they develop symptoms of heart valve disease.
It is in addition to previous guidance published by the MHRA advising that FQ’s should be avoided in non-severe infections and mild-moderate bacterial infections unless there is no alternative due to the potential for serious, disabling and potentially permanent side effects including tendonitis and neuropathy. Particular caution of FQ use is advised in certain groups including the elderly, those with chronic kidney disease, concurrent steroid therapy and those with a previous solid organ transplant.
The new potential effect of FQ’s on heart valves comes in addition to established effects of these agents on the cardiovascular system, including prolongation of the QT interval and a potential increase in the risk of aortic aneurysm and dissection.
Fluoroquinolones are recognised to be directly toxic to Type I and Type III collagen synthesis in-vitro which can manifest in-vivo as acute tendonitis (often manifesting as Achilles tendon rupture) and retinal detachment either during or shortly after their administration. Potential mechanisms include up-regulation of matrix metalloproteinases and inhibition of collagen producing fibroblasts. In addition to the Achilles tendon, Type I and III collagen also forms most of the collagen in the aortic valve, hence the plausibility that these agents could also lead to valvular insufficiency.
A recent US observational study by Etminan et al (JACC 2019) suggested that there may be a link. The analysis, based on 102 valvular regurgitation events in patients receiving FQ treatment suggested an increased relative risk of aortic or mitral regurgitation of 2.4 and 1.75 compared with those prescribed amoxicillin and azithromycin respectively. This effect was only seen in those with recent FQ administration, with the effect not observed in those with past FQ administration. The purely observational nature of the study makes firm conclusions difficult, however, these data combined with the potential mechanistic plausibility has led to the MHRA to issue this safety update. Currently, any such observational study is solely hypothesis generating, however, the impracticalities of a randomised control trial to further evaluate this mean the link is unlikely to be more formally tested.
It will therefore be important that Cardiologists are aware of this potential link and are alert to the potential valvular (and indeed aortic) complications in those receiving systemic or inhaled FQ’s.
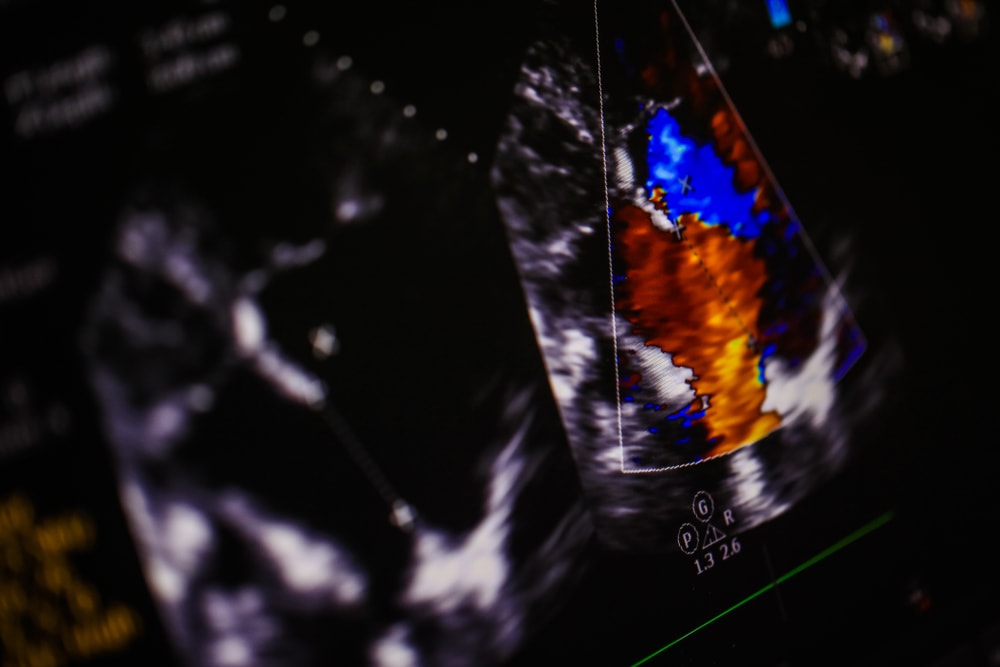
Timely access to echo in those developing signs or symptoms of heart valve disease in those prescribed systemic FQs is important given this most recent advisory, as is continued use of the MHRA ‘yellow card’ system to report potential drug complications in order to further understand this association..