By Dr Megha Agarwal
A new study1 has been published in JAMA evaluating whether there is a difference in risk of major ischemic or haemorrhagic events in patients with atrial fibrillation treated with rivaroxaban versus apixaban for stroke prevention.
Ray et al. looked at the outcomes of over half a million patients (n = 581 451) treated with either standard or reduced dose of rivaroxaban or apixaban, and found treatment with rivaroxaban was associated with a higher risk of both major ischaemic events (HR 1.12, 95% confidence interval 1.04 – 1.20), and haemorrhagic events (HR 1.26, 95% confidence interval 1.16 – 1.36), when compared to apixaban. It is hypothesised that this may be due to greater peak-through variability in rivaroxaban concentrations.
It is interesting that the rivaroxaban cohort (n = 227 572) had fewer risk factors for the study outcomes than the apixaban cohort, yet despite this, still had a higher incidence of ischaemic or haemorrhagic stroke. The difference was also more marked for the patient’s receiving reduced doses of rivaroxaban or apixaban, which is already a patient population likely to be more frail, and with more co-morbidities, thus making anticoagulation choice particularly important.
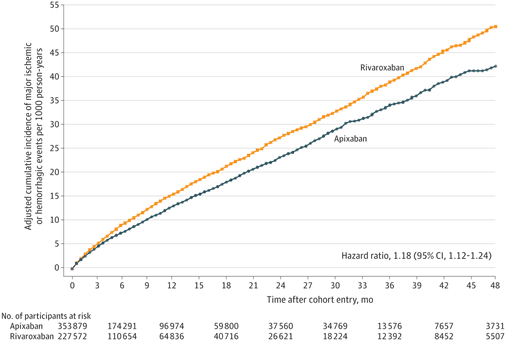
Taken from: Figure 2 of Association of Rivaroxaban vs Apixaban With Major Ischemic or Hemorrhagic Events in Patients With Atrial Fibrillation
Reference:
- Ray WA, Chung CP, Stein CM, et al. Association of Rivaroxaban vs Apixaban With Major Ischemic or Hemorrhagic Events in Patients With Atrial Fibrillation. JAMA. 2021;326(23):2395–2404. doi:10.1001/jama.2021.21222
Available from: https://jamanetwork.com/journals/jama/fullarticle/2787319

