By Dr. Ahmed El-Medany
Key points:
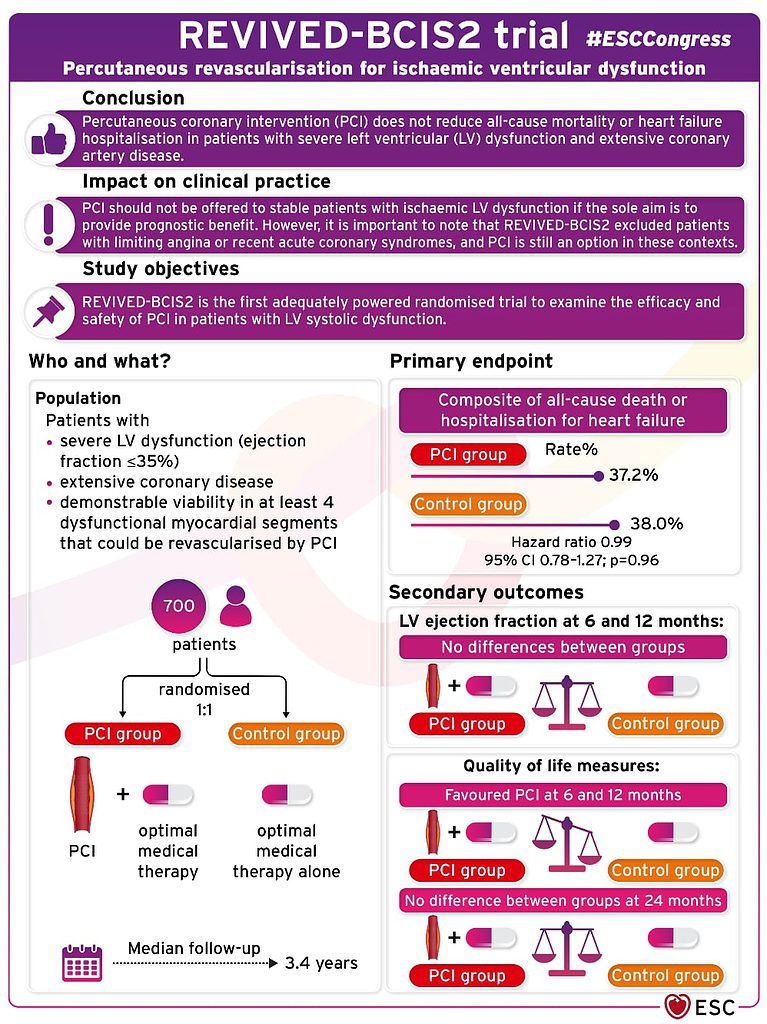
- PCI does not reduce all-cause mortality or heart failure hospitilisation ins patients with severe LVSD and extensive CAD, and PCI should not be offered to these patients with the intention of providing prognostic benefit
- REVIVED-BCIS2 excluded patients with limiting angina or recent ACS. PCI is still an option in these contexts
- REVIVED-BCIS2 is the first adequately powered RCT to examine the efficacy and safety of PCI vs OMT in patients with severe ischaemic cardiomyopathy
The results of REVIVED-BCIS2, the first adequately powered randomised trial to examine the efficacy and safety of percutaneous coronary intervention (PCI) versus optimal medical therapy (OMT) for severe ischaemic cardiomyopathy, evoked surprise and some audible groans when presented at the hot line session at ESC 2022.
Despite no randomised evidence to support PCI in severe stable left ventricular systolic dysfunction (LVSD), it is often performed in this group of patients, although is supported as a Class IIa recommendation within current European guidelines. Randomised data from the STICH trial support coronary artery bypass graft (CABG) surgery within this patient population (Class Ib).
REVIVED-BCIS2 enrolled participants with severe LVSD (ejection fraction ≤35%), extensive coronary artery disease, and demonstrable viability in at least four dysfunctional myocardial segments that could be revascularised by PCI. Viability was assessed by any modality, although cardiac magnetic resonance imaging was used most. Exclusion criteria included myocardial infarction (MI) within four weeks, decompensated heart failure, or sustained ventricular arrhythmias within 72 hours.
700 patients from 40 centres in the UK were randomly assigned in a 1:1 ratio to either PCI with OMT or OMT alone. The median age was 70 years, 88% were male, and the mean left ventricular ejection fraction was 27%. The primary outcome was the composite of all-cause death or hospitalisation for heart failure. Secondary outcomes included left ventricular ejection fraction (LVEF) at 6 and 12 months and quality of life measures.
Despite hypothesising that PCI would improve event-free survival within the patient population, lead investigator Divaka Perera (King’s College London) reported that, during a median follow up of 3.4 years, the primary outcome occurred in 129 (37.2%) patients in the PCI group and 134 (38%) patients in the OMT alone group (hazard ratio (HR) 0.99 (95% confidence interval 0.78–1.27, p=0.96))
‘The key take home message from this, where I am concerned is that this is now a definitive result, we finally have RCT evidence that allow guidelines to be strengthened on the one hand, and allow clinical practice to be rationalised around the world on the other,’ Perera announced.
There was no significant difference seen between groups regarding LVEF at 6 and 12 months. Quality of life favoured PCI at 6 and 12 months but no difference was seen between groups at 24 months. Asked about the quality of life results in the press conference, Perera explained that more data on this will support a health-economic analysis of the trial data.
In conclusion, REVIVED-BCIS2 suggest that PCI does not reduce all-cause mortality or heart failure hospitilisation in patients with severe LVSD and extensive coronary artery disease, and should not be offered to stable patients with ischaemic LV dysfunction if the sole purpose is to provide prognostic benefit. Nonetheless, it is important to note that REVIVED-BCIS2 excluded patients with limiting angina or recent acute coronary syndromes, and PCI is still an option in these contexts.
Figure 1: Pictorial summary of REVIVED-BCIS2. Sourced from the European Society of Cardiology Twitter feed (@escardio).
Read the full study in NEJM: https://www.nejm.org/doi/pdf/10.1056/NEJMoa2206606

