By Guy Lloyd
In one of the standout session during BCS 2021, the enormous problem of cardiologist burnout, its causes and consequences as well as potential strategies to address the issue were discussed.
In the concluding remarks it was noted that none of the panellists (which included the Presidents of the British Cardiovascular Society (BCS) and Irish Cardiac Society (ICS), the current and past presidents of to American College of Cardiology (ACC) and the Director of Health and Wellbeing for the RCPI) could imagine such a session happening 20 years ago, but all agreed that burnout symptoms and their consequences were a particular problem for cardiologists.
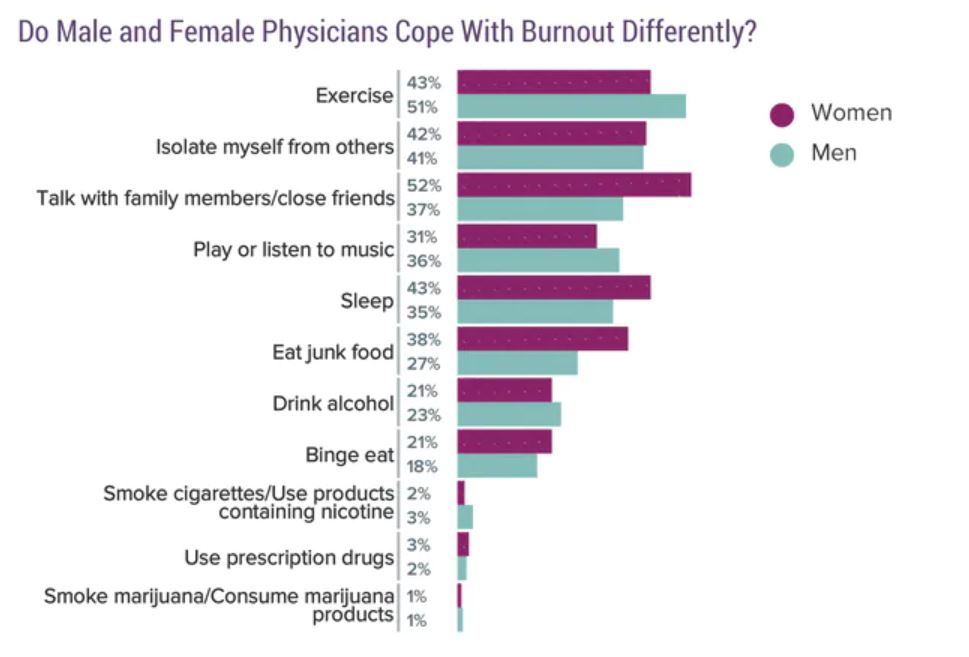
The nature and causes of burnout were extensively discussed and in particular how it impacts individual health and wellbeing, through biological changes such as hypertension and increased cortisol levels, maladaptive behaviour such as disordered eating, drug and alcohol abuse, and more social consequences such as isolation and relationship breakdown. Terrifying figures for the excess risk of suicide (a 40% higher risk in men and 130% in women!)
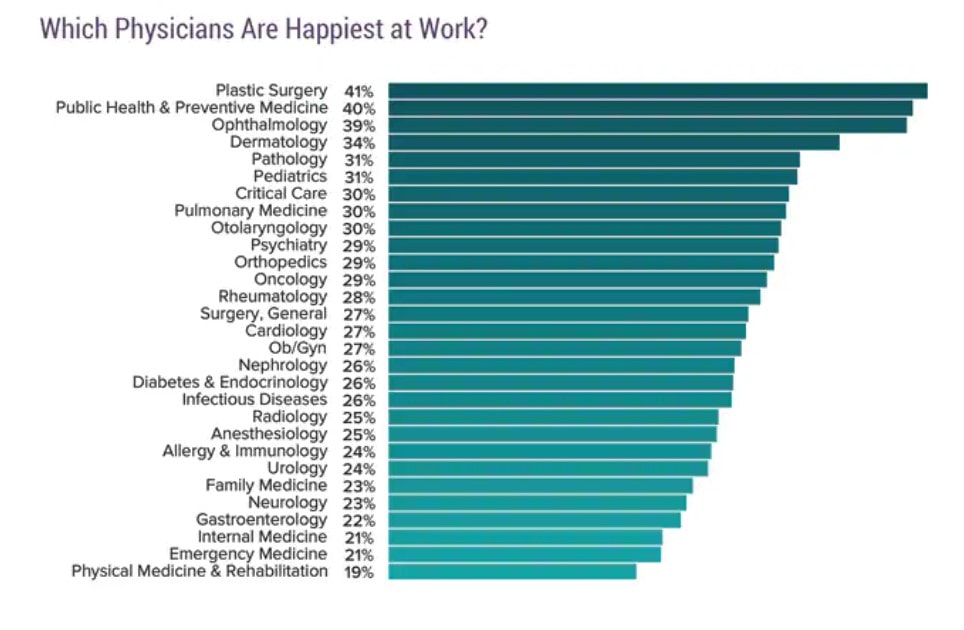
The scale of problem is also difficult to comprehend with between 40% and 70% of US clinicians expressing burnout symptoms and 15% frank depression, but only 13% seeking professional help. Cardiologists are at the bottom of the league table both for happiness in job, and for seeking help.
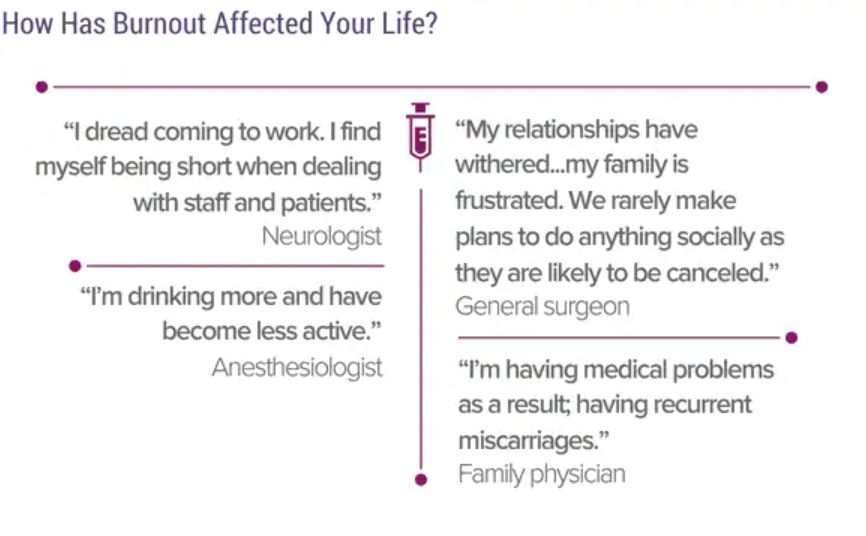
Burnout is clearly bad for patients with reduced effectiveness and efficiency as well as an increase in medical mistakes. Perhaps most importantly the emergence of an empathy gap which patients really notice!
And all of this before COVID-19 which as an unexpected stressor, reducing professional control and further separating the relationship between professional satisfaction and trying to do a good job, has doubled the risk of burnout
Solutions and mitigations were discussed, self knowledge, self awareness, mentorship and professional coaching ( a relatively alien concept in the UK) all have a major role. Programs such as the Mayo Clinic Nine Step model allow systems and institutions to build a culture of wellbeing and resilience.
The key requirement for all of us, and especially those in leadership positions, to look at our colleagues, give them space to express authentic feelings and concerns and build this into our usual ways of working, was emphasised. “Change one thing a year” and in time you have changed a lot.
This session at BCS2021 is a wake up call which the BCS takes incredibly seriously and will champion in the years ahead. Many thanks to the participants:
Prof Simon Ray
Prof Vincent Maher
Prof Gaye Cunnane
Dr Dipti Itchhaporia
Dr Mike Valentine
Image Credits/References: Medscape National Physician Burnout, Depression & Suicide Report 2019: https://www.medscape.com/slideshow/2019-lifestyle-burnout-depression-6011056#11